PNNL Coronavirus Research Unlocks Clues for Fighting COVID-19

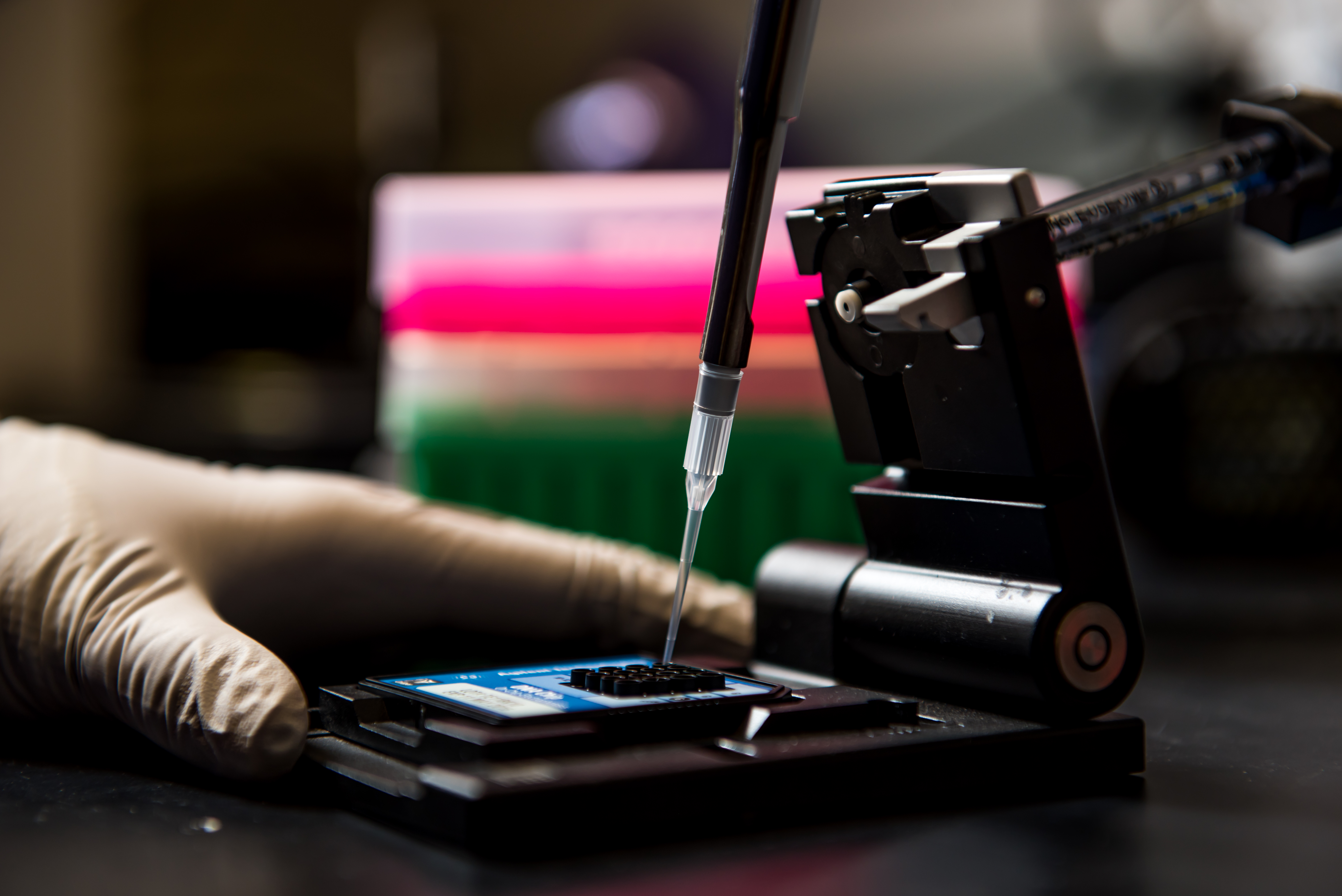
PNNL biomedical scientist Jennifer Kyle and her colleagues investigate viruses to better understand how they live and thrive on host cells.
(Photo by Andrea Starr | Pacific Northwest National Laboratory)
Two years ago, the first case of COVID-19 emerged in the United States, right here in Washington state.
As soon as the pandemic reared its head, scientists, including those at the Department of Energy’s Pacific Northwest National Laboratory, focused on learning about the virus that causes COVID-19 so it could be better detected, treated and prevented.
PNNL’s research on coronaviruses began long before COVID-19 was the topic of daily discussion.
As part of a collaboration with the University of North Carolina at Chapel Hill, PNNL scientists began a study of the coronavirus that causes Middle East Respiratory Syndrome, or MERS, nearly a decade ago.
While MERS is not as common or contagious as COVID-19, it is more lethal and has the potential to become a pandemic of its own.
The MERS coronavirus (MERS-CoV) is related to severe acute respiratory syndrome coronavirus 2 (SARS-CoV 2) that causes COVID-19.

So, studying MERS-CoV may one day lead to better treatments for a host of respiratory illnesses, including the many variants of COVID-19.
Like SARS-CoV 2, MERS-CoV attacks the lungs. As researchers deepened their understanding of how MERS-CoV damages the lungs of infected patients, they found clues that could help stop it.
Their early results are promising, including the development of an approach for treating coronavirus infections using a compound that targets a cellular enzyme the team identified.
Scientists are now seeking ways to optimize this antiviral compound and to confirm its effectiveness.
Researchers began their study by investigating what causes certain cells in the lungs to succumb to MERS-CoV infection.
In the laboratory, they analyzed tens of thousands of measurements of specific proteins and other indicators present in lung tissue after an infection.
They subsequently narrowed in on one of the enzymes associated with the molecular process that causes the infected cell to call “time out” in response to a MERS-CoV infection.
Proteins are responsible for the function and regulation of processes in our cells, tissues and organs. For a variety of reasons, including response to infection, our bodies can start making faulty proteins.
When that happens, a quality-control function kicks into action. Cellular activity shifts from producing new proteins to making emergency repairs.
If the faulty proteins can’t be repaired fast enough, other proteins are sent in to euthanize the cell.
Scientists discovered that this mechanism of shifting from protein building to protein repair, and ultimately cell death, is highly active in certain lung cells infected with MERS-CoV.
This led them to identify a compound that might block the enzyme responsible for initiating this process—stopping it from occurring and preventing resulting lung damage.
Laboratory tests at the University of North Carolina showed that the compound stopped virus replication in human lung cells and boosted lung function and reduced lung damage in mice infected with MERS-CoV.
MERS-CoV attacks different lung cells and settles deeper in the lungs than the virus that causes COVID-19.
So, while the approach for combating MERS-CoV may not be directly applicable to COVID-19, improving the understanding of how our bodies respond to one coronavirus may help us find new ways to treat and prevent the one that has killed more than 900,000 Americans.
Decades of research on the human immune system and its response to coronaviruses served as the foundation for the quick development of COVID-19 vaccines.
These vaccines have proven to be safe and effective in protecting against infections and reducing the risk of severe illness and death.
Additional research, such as this MERS project, will no doubt prove equally beneficial as we encounter new variants of COVID-19 and other coronavirus-induced diseases.
COVID-19 is not yet done with us, but as I look beyond the pandemic with cautious optimism, it is heartening to know that PNNL scientists and many others are pushing the frontiers of science to deliver medical advancements that will benefit us all.
Steven Ashby, director of Pacific Northwest National Laboratory, writes this column monthly. To read previous Director's Columns, please visit our Director's Column Archive.
Published: February 21, 2022