Fentanyl Analogs
What are fentanyl analogs?
Fentanyl analogs are illicit—and often deadly—alterations of the medically prescribed drug fentanyl. The analogs have similar—but not the same—chemical structure, and they mimic the pharmacological effects of the original drug.
Fentanyl is a very strong synthetic narcotic primarily used to ease the suffering of patients with chronic pain or terminal illnesses. Since the 1990s, the drug has been available in a patch or lozenge for easy and effective delivery of the time-released medicines. Fentanyl is so potent that residual chemicals in used patches have been suspected of contaminating water supplies when flushed down the toilet. Used patches have also been known to stick to children or animals, causing unintentional overdoses.
But accidental overdoses from legal prescriptions pale in comparison to deaths attributed to illegally imported versions of the drug and its analogs starting in the late 1990s. The effectiveness of the drug, combined with user-friendly delivery methods, drew the attention of bad actors seeking to profit from its potency.
Take heroin, for example. In the height of the opioid epidemic, a kilogram of heroin could be purchased for approximately $6,000 and sold for appropriately $80,000. For the same purchase price, a kilogram of illegally imported fentanyl could be sold for approximately $1.6 million, then cut into heroin and other drugs to expand their volume.
Some black-market drug makers create new fentanyl analogs to avoid classification as illegal, get around policy restrictions on manufacturing, and evade detection in standard drug tests. It can be difficult to determine if pills were legally produced for pharmaceutical distribution or illegally produced for illegal drug sales. Counterfeit prescription medications, such as a fentanyl-laced Xany-bar or counterfeit Xanax, were reportedly made at a “pill mill” or illegal pill press.
The availability of black-market fentanyl and fentanyl analogs led to a U.S. opioid epidemic that continues to cause thousands of overdose deaths each year and destroy families and communities in the process. Harm from fentanyl analogs also extends to first responders. A lethal dose of carfentanyl, a fentanyl analog, is about the size of the head of a pin, requiring the full protection of hazmat suits.

History of fentanyl analogs
Fentanyl was created in 1959 by Dr. Paul Janssen as an intravenous surgical analgesic. The drug is 50–100 times more potent than morphine. Because of its strength, the drug was rarely used except in hospital operating rooms or on large animals.
In the 1990s, a new transdermal skin patch for fentanyl was developed to treat chronic pain. The non-surgical delivery mechanism offered some unique advantages over other drugs, including quick onset of action, relatively few cardiovascular risks, and low histamine release. These attributes made it a good prescription choice for some patients, because it reduced some of the risks of medical complications that other pain relievers have.
Lozenge, lollipop, tablet, and nasal spray versions soon followed, under such names as Actiq®, Duragesic®, and Sublimaze®. The ease and effectiveness of these user-friendly delivery methods led to abuse, and the fentanyl analog market was born. Criminal manufacturers began creating designer drugs—analogs with modified chemical structures—to avoid identification as a controlled substance.
From 1999 to 2011, the death rate in the United States due to opioid analgesics nearly quadrupled, then began to skyrocket around 2013–2014. This timing coincided with the first detection of illicit pills containing fentanyl, fentanyl analogs, and other novel synthetic opioids such as U-47700.
Warning signs of the fentanyl-fueled opioid crisis first emerged in the Northeast. William R Brownfield, Assistant Secretary for the Office of National Drug Control Policy, warned that Massachusetts was “a preview of coming attractions.” Across the United States, drug abuse, addiction, and overdoses were responsible for 50,000 deaths in 2015, the majority of which involved an opioid.
In 2017, the President issued Executive Order 13784, establishing a Commission on Combating Drug Addiction and the Opioid Crisis. Many of the 45,000 drug-related deaths that year were determined to have resulted from abuse, addiction, and overdoses due to fentanyl.

Unflooding the fentanyl analog market
A major contributor to the opioid drug crisis was availability. Modern internet e-commerce enabled individual players, small-scale drug trafficking organizations (DTOs), and large-scale DTOs with their own production facilities to flood the illicit drug market with fentanyl. The drugs could be purchased and delivered through standard mail to the United States from places as far away as China. In many cases, drug users and mid-level dealers have no idea where or how their drugs are manufactured or what they might be cut with.
Carfentanyl, a fentanyl analog, is an odorless white powder. It is one of the most potent opioids known and used commercially. According to the National Institute on Drug Abuse, carfentanyl is approximately 10,000 times more potent than morphine, 100 times more than fentanyl, and 50 times more than heroin. Marketed under the trade name Wildnil®, it is used as a general anesthetic for very large animals.
In July 2016, carfentanyl was found cut into heroin and fentanyl sold on the streets of Ohio. In a span of three days, 35 overdoses and 6 deaths occurred there. In the same year, in Anoka County, Minnesota, six overdoses and two deaths occurred in a 12-hour period in October 2016. These instances and similar cases throughout the nation pointed to single batches of fentanyl-laced heroin as the culprit for dramatic spikes in overdose cases.
Most opioid users do not intentionally seek out fentanyl analogs. To unsuspecting customers, the drugs can look like legal opioids or benzodiazepines for pain relief. And once a person is exposed to a higher-toxicity drug, the brain chemistry alters further, and the user will seek out the most potent form of the drug. At the height of addiction, some users are unable to discern risk and are willing to go to any length to obtain the drug, including boiling fentanyl patches to extract the drug for injection or ingestion. And if a user is new to taking opioids, the risk of overdose is even higher because their bodies have no tolerance to the drug.
Fentanyl analogs, including fentanyl-laced heroin, come in many flavors, with street names such as white heroin, Perc-O-Pops, Chiclets, Apache, China Girl, White China, Dance Fever, Jackpot, Murder 8, TNT, Tango and Cash, Friend, Goodfella, and Redrum (murder spelled backward). The sheer variety of the drug, including emerging combinations, make toxicology testing and accurate death reporting extremely challenging.
Investigations into drug overdoses have shown the difficulty in identifying whether drugs were commercially or illegally produced. For example, carfentanyl and other analogs do not show up on traditional opioid toxicology testing. And specific testing for these substances is not routinely performed. An investigation may show all the scene indications and autopsy findings of an opioid overdose death, but simple toxicology tests can still be negative for opioids. in many states, medical examiners are often too overwhelmed by the numbers to do the testing to determine which analog was involved.
The toll of drug abuse and overdoses extends far wider than deaths, which in 2019 reached nearly 50,000. The costs to families, communities, and emergency response in terms of dollars, psychological, and health effects are incalculable. Nipping the problem in the bud—keeping illicit drugs from reaching the market—is critical for stemming the tide of illegal drug activity and protecting the nation from the scourge of fentanyl analogs.
As part of the federal response to EO 13784, the Department of Homeland Security’s Science and Technology Directorate established a collaboration among U.S. Customs and Border Protection (CBP), the United States Coast Guard, other federal agencies, and first responders. Their goal is twofold: (1) to identify and develop improved fentanyl detection capabilities, including standards and advanced rapid detection technologies and analytics, and (2) to increase capacity to disrupt the supply of drugs being smuggled into the United States.

Challenges of fentanyl analogs
Synthetic opioids present immense challenges to detection, particularly in the vast infrastructure that enables speedy and high-volume legitimate trade. From shipping docks and airports to border crossings and mailrooms, smugglers go to great lengths to hide their drugs in the flow of legal commerce.
Dogs with their keen sense of smell have been trained for a variety of U.S. security and emergency response settings for more than 50 years. The first drug-sniffing dogs were put into service in the mid-1960s and are now regularly seen in cargo terminals, airports, mail delivery and sorting centers, and even schools.
But training and maintenance associated with sniffer dog teams is expensive. And dogs and their handlers can only take so much. They can get burned out, or worse, suffer health effects from the chemicals and fumes associated with illicit drugs such as fentanyl analogs. Even a minute amount of drug-to-skin contact can be deadly.
In the last decade, technologies for chemical detection have been developed to try and replicate the sensitivity of a dog’s nose. In a dog, the part of the brain used to detect and analyze smells is also about 40 times more efficient than humans.
Specialized laboratory equipment and analytical techniques such as GC-MS (gas chromatography mass spectrometry) and LC-MS/MS (liquid chromatography tandem mass spectrometry) can identify regulated fentanyl compounds. As emerging new compounds appear on the market, nontargeted testing can be aided with LC-HRMS (liquid chromatography high-resolution mass spectrometry).
But it is one thing to test samples in a laboratory, using known spectra libraries and large instruments. The testing process also takes time—too much time for a field setting.
Two early models of handheld chemical analyzers, or spectrometers, came out in quick succession. TruNarc debuted in 2012, followed by TacticID in 2014. The compact, lightweight, and robust devices have simple push button controls and work by scanning. For illicit or dangerous substances such as fentanyl, heroin, cocaine, or methamphetamine, the screen turns red. Drug precursors or chemicals that can mask some narcotics’ Raman signals return a yellow or orange screen. Green means all clear.
In 2019, SwabTekTM introduced new field kits with dry test strips capable of detecting fentanyl and other dangerous narcotics. The single-use recyclable spot test uses a paper strip with dry reagent test zones applied to the strip surface. A cotton swab is used to transfer the suspect residue to the paper strip test zone. The SwabTek test kits provide a safe, 100% recyclable, non-hazardous alternative to the industry standard “wet chemistry” field kit.
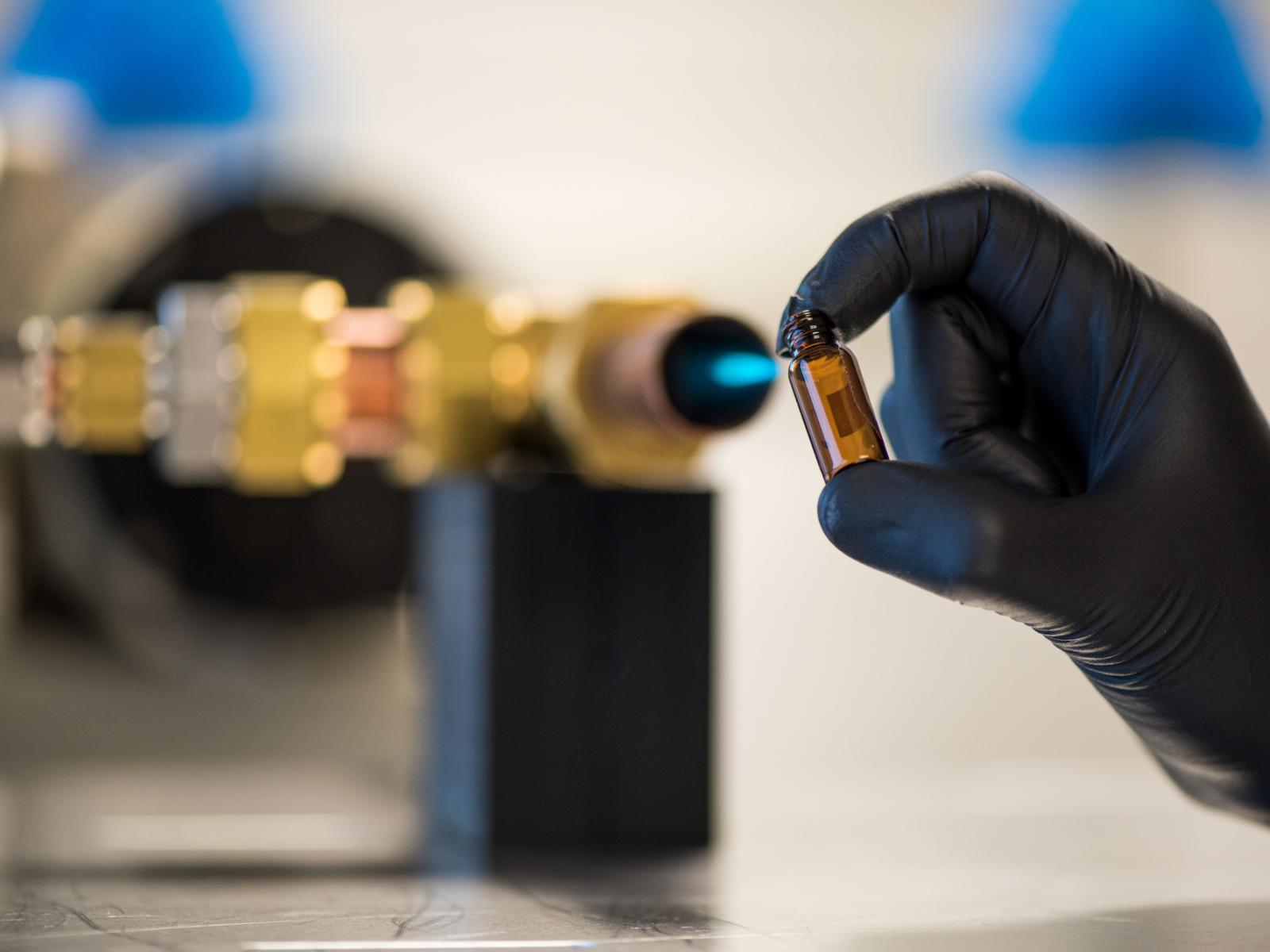
Field technologies such as the ones described above require close contact to the sample source. One example of a new standoff detection technology is Pacific Northwest National Laboratory’s (PNNL’s) ultrasensitive vapor detection system, VaporID. Rather than searching for particle residue using surface swipes or pulses of air to dislodge particles for analysis, the system 'sniffs' for vapors, much the way canines do.
VaporID joins an atmospheric flow tube with a mass spectrometer. The system can accurately detect organophosphorus compounds and narcotics at ultra-low levels previously impossible to detect in the presence of other chemical vapors. The technology could complement or replace contact and canine-assist detection methods for drug screening used in mailrooms, airports, and shipping centers.
Improving detection of fentanyl analogs
Unscrupulous scientists persist in exercising their craft, working in underground labs to manipulate fentanyl, isolate analogs, and create deadly combinations. The collection of hard-to-trace substances entering the market continues to kill users and sicken law enforcement as they battle the epidemic.
The Department of Homeland Security (DHS) has a significant role in countering the trafficking of opioids and other narcotics into the United States, including detection and interdiction of illicit narcotics, as well as investigative efforts to disrupt and dismantle smuggling operations. The DHS Science and Technology Directorate Opioid Detection Program supports the mission requirements of CBP, Immigration and Customs Enforcement Homeland Security Investigations (ICE HSI), and state/local law enforcement in four primary areas:
- High-throughput, nonintrusive screening technologies to rapidly and automatically identify anomalous and suspected concealed narcotics
- Automated alarm resolution technologies to provide confirmation of opioids and other narcotics, without having to physically open or handle the shipment
- Improved effectiveness of handheld detection systems employed by frontline operators to detect small amounts of drug materials, even when diluted
- Advanced analytical tools for analysis of evidence, data fusion, and information sharing to enable automated detection.
In January 2021, DHS announced a new multiphase study to improve the detection of synthetic opioids. In collaboration with PNNL, the study will assess the performance of field-portable drug detection equipment from industry against fentanyl and fentanyl-related compounds, other drugs, and cutting agents.
For the study, the industry partners will obtain the latest reference spectra for approximately 50 DEA-controlled substances, including novel synthetic opioids, as well as independent test results, which will enhance their capability and marketability. End users of the equipment—the first responder and interdiction communities, as well as interested federal, state, and local agencies—will also benefit by receiving system updates with the expanded libraries at no cost. They will gain a broader understanding of the capabilities and limitations of current field detection equipment to feel more secure with detection performance.
The effort specifically targets instruments used by federal, state, local, tribal, and territorial law enforcement and first responders that use spectral libraries to identify unknown samples suspected of containing illicit drugs. These include, but are not limited to, field-portable gas chromatograph/mass spectrometers, high-pressure mass spectrometers, ion mobility spectrometers, Raman spectrometers, and Fourier transform infrared spectrometers.
In the coming years, DHS will continue partnering with industry to complete narcotics data collection for government-owned spectral libraries and will initiate a new Opioid Investigation and Intelligence Project to support ICE HSI.
Fentanyl analogs research at PNNL
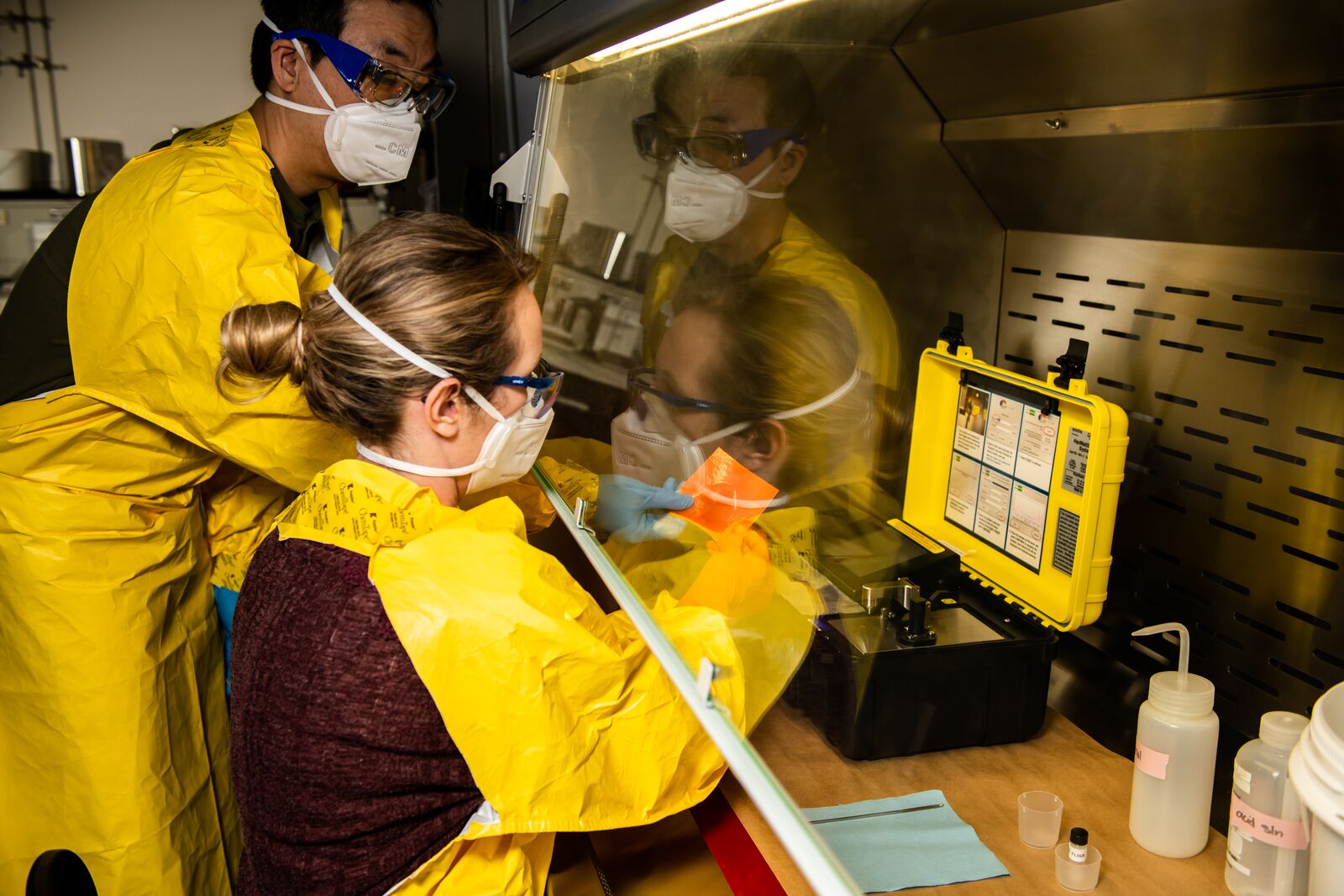
At PNNL, teams of biologists, chemists, and engineers work every day to solve challenges related to chemical and biological detection and forensics. This multidisciplinary approach supports important national security missions, including the development, integration, and evaluation of methods to detect biomolecules such as illicit drugs.
Rich Ozanich is a PNNL project manager of opioids standards and equipment testing. In June 2021, he kicked off the DHS S&T Directorate’s Whole-of-Government Virtual R&D Showcase as part of an expert panel discussion, “Opioids Detection and Partnerships: Responding to a Public Health Crisis.” The panel highlighted PNNL’s partnership with DHS S&T, industry, and communities to improve detection of synthetic opioids toward stronger and more resilient communities.
As part of that partnership, PNNL’s fentanyl handling and detection experts are helping assess the performance of detection equipment used by emergency responders. The work informs standards and tools for quickly detecting fentanyl and its analogs. Advances in both these areas aim to reduce the exposure of dangerous drugs to emergency responders.
Kristin Omberg, leader of PNNL’s Chemical and Biological Signatures group, worked with fellow subject-matter experts on the Biodefense Policy Landscape Analysis Tool. Unlike any other product of its type available, the tool captures relevant biodefense policy directives and sections of the U.S. Code in a format conducive to visualization. Launched in 2018, it was designed to help the government understand the current state of the U.S. biodefense enterprise.
Building on that work, Omberg and her team also developed the National Response Framework Policy Landscape Analysis Tool for the Federal Emergency Management Agency. The visualization tool, debuted in March 2021, lays out the United States’ strategy for responding to any type of emergency. It parses the framework’s requirements and elements in the form of icicle and sunburst charts.
Robert Ewing is a chemist at PNNL and the lead inventor of the VaporID technology, which was named Geekwire’s Innovation of the Year in 2019. Before a public version hits the streets—or the airport, or the mailroom, or any number of places where public safety is imperative—portability and integration into existing screening methods are key hurdles that need to be overcome.
These are just a few examples of collaborations between PNNL experts and DHS, industry, and communities to improve detection equipment and methods used by emergency responders to sniff out fentanyl analogs and other dangerous opioids.
